An Invisible Work Hazard Affects GI Staff
by Chad Griepentrog, on May 03, 2019
Nurses are often exposed to a number of potential environmental hazards when performing their jobs. On a daily basis, we encounter patients who need our assistance to keep from falling while ambulating, require a helping hand with toileting needs, need an intramuscular injection, or have a dressing that needs changing. All of these tasks, which nurses around the world might perform multiple times during a typical shift, carry an inherit risk that could expose the nurse to injury or infection. Although the majority of us are able to perform these routine nursing duties without a second thought, it only takes one misstep or unusual circumstance to cause harm to the nurse. Unfortunately, when exposures, patient falls, or other incidents occur, they can have long-term physical effects on the nurse/technician.

For those of us in the field of GI nursing, we have our own unique risks that we may encounter on a daily basis as a part of doing the work we love to do. One such hazard that I was reminded of recently was radiation exposure. As a healthcare professional for the past 18 years, I have encountered my share of radiation exposure through my work with patients at community hospitals. Over the last seven years of working in endoscopy, the majority of this now comes through procedural work with our advanced endoscopy providers, providing therapeutic services via ERCP; stenting of the colon, esophagus, and duodenum; and performing complex dilations. Left unchecked, this daily fluoroscopic exposure has the risk to do harm and can have long-term health effects. Consequences to GI nurses and technicians as well as radiology technicians, endoscopy physicians, and anesthesia providers could include damage to the skin and the lens of the eye, and even cellular damage that may lead to cancer.

Fluoroscopy table
As beneficial as this imaging technology can be, we must also use it judiciously to prevent harm to our patients and one another. Fortunately, we know that there are several things that can be done to minimize our exposure to radiation scatter. The one thing that most of us think of is wearing a lead apron or wrap to block the ionizing energy from reaching our vital organs and sensitive glands. Although not always possible, we can also minimize our exposure by increasing our distance from the radiation source (e.g., C-arm). Our providers can also help by using the lowest level of magnification needed and limiting the time that images are being captured.
At our hospital, our department leadership has taken additional steps to ensure we are keeping our staff safe.
- Members of our advanced endoscopy team were recently custom-fitted for their own lead aprons and thyroid guards. Staff were able to pick out the style that was most comfortable for them and provided protection but was considerably lighter weight than the aprons we had been wearing previously for lengthy procedures.
- Several years ago, I brought forward concern over the length of some of our complicated procedures and wanting to also protect my eyes. Our team was then given the option to choose from several styles of lead-lined safety glasses, which most of us took advantage of.
- Our institution has yearly radiation safety education that is mandatory for all nursing staff.
- A policy is in place that requires investigation from leadership and safety personnel in the unlikely event that there is a procedure where more than 60 minutes of fluoroscopy is used.
- All of our staff wear dosimeter badges on the outside of their lead to monitor exposure limits, and all pregnant females are encouraged to wear neonatal dosimeters under their lead attire as well.
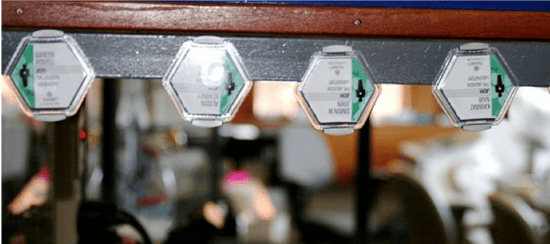
Dosimeter badges
These are all safeguards that should be commonplace to protect ourselves from an otherwise silent and invisible hazard in our work environments.


