COVID-19 and Colonoscopy: Considerations for Endoscopy Staff
by ColoWrap, on April 29, 2020
Colonoscopy is a high-touch procedure that has always placed staff at some risk for infections, but how have things changed since the onset of the COVID pandemic? Currently, in most areas of the country, non-essential procedures like colonoscopy are on hold. However, when social distancing restrictions are lifted and the hiatus is over, a backlog of patients will require endoscopic procedures. How can staff, physicians, and patients all stay safe?
A COVID Primer
If you don’t know by now, COVID-19 is a respiratory disease that spreads readily among individuals. It is caused by the coronavirus, which circulates through droplets in the air and can remain viable on surfaces for hours to days. The virus can be transmitted through coughing or sneezing; it then enters the body through the mouth, eyes, or nose.

People infected may exhibit no symptoms at all or may experience severe medical complications, for instance, pneumonia. Older adults or people with existing chronic medical conditions are at greater risk of becoming seriously ill. An estimated 5.7% of people infected with the virus in the US have died. Because it is easily spread from person to person, WHO and the CDC warn against close contact (within about 6 feet) with anyone who is sick or has symptoms. The problem is, it is not easy to tell who is infected. In fact, a recent study in the British Journal of Medicine concluded that 78% of people with COVID-19 exhibit no symptoms.
COVID and Upper Endoscopy
According to the ASGE, during upper endoscopy procedures, physicians and staff are exposed to splashes, mucus, and saliva. Specifically, patients often cough as the scope is inserted and removed and during procedures. Given the close contact among patients, doctors, and staff and the fact that the virus is transmitted through aerosolized droplets, upper endoscopy procedures conducted without or with minimal personal protective equipment (PPE) are a perfect environment for spreading the virus.
Colonoscopy in the COVID Era
Performing or assisting with colonoscopy was initially considered lower risk for coronavirus transmission, but recent evidence has emerged that disproves this theory. One study found that the virus can be transmitted through fecal matter and that viral RNA can persist in feces for up to 47 days after respiratory samples test negative. Furthermore, when air or carbon dioxide is insufflated to improve visualization of the colon, the patient expels excess gas via the mouth or anus. Considering that the average speed of flatulence leaving the body is 10 feet per second, staff assisting with colonoscopy are routinely exposed aerosolized biological samples.
How to Stay Safe During Colonoscopy
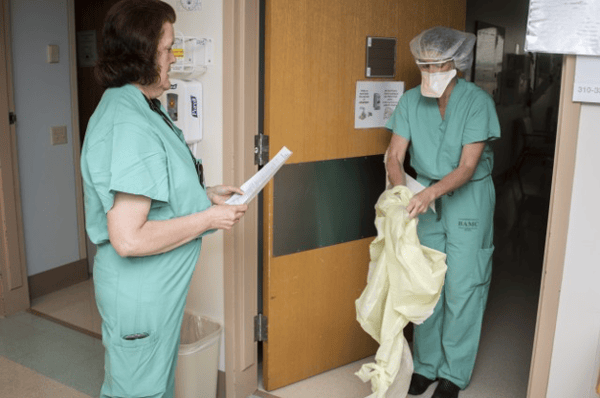
Safety recommendations for endoscopy staff include wearing full PPE, including an N95 mask; practicing strict physical distancing; and minimizing the number of people in the procedure room. While these safeguards make good sense, they are not always feasible, especially in the context of colonoscopy. First of all, there is a dearth of PPE in the U.S. The CDC stated that, “PPE shortages are currently posing a tremendous challenge to the US healthcare system because of the COVID-19 pandemic.”
Second, colonoscopies involve person-to-person contact. Nurses and technicians routinely apply manual pressure on patients’ abdomens and/or reposition patients during the procedure.
Not only are staff who assist with colonoscopy at risk for musculoskeletal disorders, they are more likely to contract COVID. Routine tasks like applying abdominal pressure put one or more staff well within six feet of patients’ aerosolized materials for a prolonged time. In addition, the physical demands of these duties increase the respiration of staff performing them. This is could potentially increase the degree of exposure.
ColoWrap Protects Against Injury…and (Potentially) Coronavirus
Now, more than ever, it is essential to minimize patient contact during colonoscopy to protect staff.
ColoWrap is the only clinically proven solution designed to eliminate the need for staff applied manual pressure and patient repositioning during colonoscopy. ColoWrap delivers sustained, adjustable pressure to splint the patient’s sigmoid and transverse colon, resulting in a 90% reduction in the need for staff applied manual pressure and patient repositioning, quicker and easier scope advancement, and better procedure outcome. And because staff are not applying manual pressure repositioning patient, they are able to maintain a safe physical distance during the exam.
 Well before COVID, endoscopy professionals were aware of the importance of infection control. In the current environment, additional measures must be taken to protect staff. If possible, PPE should be worn during every endoscopic procedure, and social distancing should be practiced. In addition, using ColoWrap can help to limit patient contact during colonoscopy; it’s an easy way to keep staff safe during colonoscopy. Click below to learn more about how to implement ColoWrap in your unit as you restart procedures.
Well before COVID, endoscopy professionals were aware of the importance of infection control. In the current environment, additional measures must be taken to protect staff. If possible, PPE should be worn during every endoscopic procedure, and social distancing should be practiced. In addition, using ColoWrap can help to limit patient contact during colonoscopy; it’s an easy way to keep staff safe during colonoscopy. Click below to learn more about how to implement ColoWrap in your unit as you restart procedures.



